Monkeypox is a viral disease caused by the monkeypox virus, similar to smallpox but not as severe. Smallpox was eradicated in 1980, and its vaccine use stopped, making monkeypox the primary orthopoxvirus. It is mostly found in Central and West Africa, particularly in tropical rainforests. The first human case was identified in 1970 in the Democratic Republic of the Congo. Since then, it’s been recognized as endemic in these regions, with several African countries reporting cases.
Monkeypox was first noticed in monkeys in Africa in 1958. People infected with it develop small lesions or pox on their bodies, resembling symptoms of smallpox. The monkeypox virus belongs to the Poxviridae family, causing diseases like cowpox and smallpox. Monkeypox is different from smallpox despite belonging to the same genus.
The infection can spread from animals to humans and between people, but the death rate is lower compared to smallpox. Africa has a fatality rate of about 1 to 15% for monkeypox, with children experiencing a higher rate of 15 to 20%. Large rodent populations in Africa contribute to its endemic status, unlike smallpox, which only affected humans.
Transmission usually occurs through direct contact with an infected animal or consuming improperly cooked meat from infected rodents or monkeys. The virus can spread between people through respiratory droplets, though this is rare. Studies show family members can transmit it to each other in about 8 to 15% of cases.
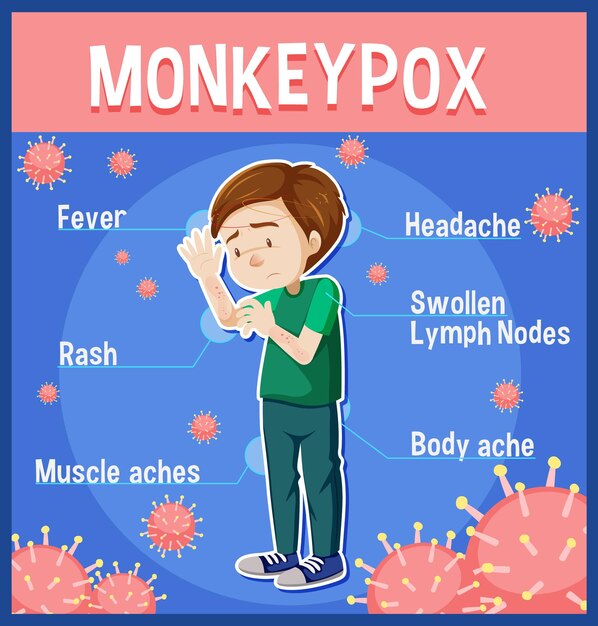
Monkeypox is caused by the orthopoxvirus genus, featuring a unique structure with a lipoprotein layer. The incubation period ranges from 6 to 13 days, with symptoms manifesting in two distinct phases. Initially, fever, headache, muscle aches, swollen lymph nodes, and fatigue occur. Afterward, a rash appears, starting on the face and spreading to other parts of the body. The rash evolves through several stages before scabbing over and falling off.
The disease typically lasts 2 to 4 weeks, with more severe symptoms in children. Risk factors include direct contact with infected animals or people and consuming meat from infected animals. Close physical contact, especially without proper protection, increases the risk of transmission within families.
Complications from monkeypox can include secondary infections, sepsis, vision loss, encephalitis, and bronchopneumonia. The fatality rate is generally low but higher among young children and those without immunity from smallpox vaccination, discontinued after smallpox eradication.
Currently, there is no specific treatment for monkeypox, but smallpox vaccination can offer significant protection. While the original smallpox vaccine isn’t widely available, a new vaccinia-based vaccine was approved in 2019 but is not yet broadly accessible. The CDC recommends measures such as smallpox vaccination within two weeks of exposure, using specific antiviral medication for severe cases, and supportive treatments.
Diagnosis is done through physical examination and laboratory tests, but due to rarity outside Africa, it requires close cooperation with health authorities. Laboratory tests like ELISA, PCR, and Western blot are used to confirm the virus.
Several animal species, including rodents and primates, are natural hosts of the virus. Preventive measures include avoiding contact with sick animals, thorough cooking of animal meat, and using protective gear when caring for infected persons. Restricting the trade of potentially infected animals is crucial to prevent global spread. Countries are implementing policies to manage this risk effectively.
Creating public awareness and educating on prevention are key strategies against monkeypox. People at higher risk, such as lab and healthcare workers, should be prioritized for vaccination. By following these guidelines, the spread of monkeypox can be controlled, and those infected can receive timely treatment.