Since the early 1990s, many advancements have been made in both the prevention and treatment of HIV/AIDS. Today, people diagnosed with HIV are living longer and healthier lives. However, HIV remains a significant public health issue in the U.S., with over 31,000 Americans receiving a positive diagnosis in 2022, according to the CDC. The good news is that HIV is entirely preventable with the right strategies.
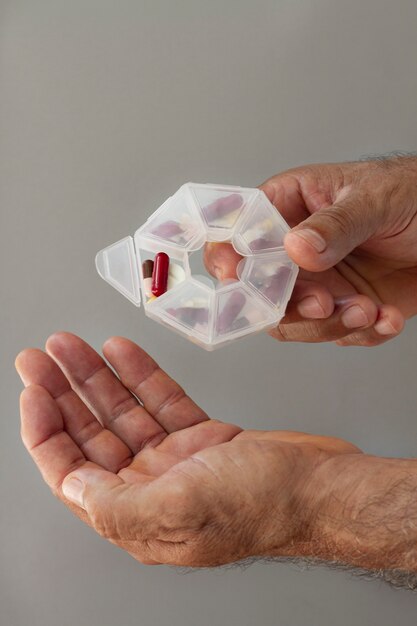
One of the most effective prevention options available is pre-exposure prophylaxis, or PrEP. PrEP refers to daily medications that reduce the risk of contracting HIV. When combined with safe sex practices, PrEP lowers the risk of sexually transmitted HIV by about 99%, and for people who inject drugs, the risk is reduced by 74%. Despite its effectiveness, stigmas, lack of awareness, and misinformation can make it less accessible to people who need it most.
PrEP is specifically designed for HIV-negative individuals to prevent infection. The medication, taken daily, works by stopping HIV from taking hold and spreading in the body, keeping users HIV-negative. There are three FDA-approved PrEP options: Truvada, Descovy, and Apretude.
– **Truvada** is available in pill form and is suitable for anyone at risk through sexual activity or injection drug use.
– **Descovy** is another pill option but isn’t recommended for individuals assigned female at birth who are at risk through receptive vaginal sex.
– **Apretude** is a newer option and is administered via injection every two months. It’s approved for anyone at risk through sex who weighs at least 77 pounds.
Descovy is a newer version of Truvada that uses a smaller dose of one ingredient, which helps reduce certain side effects. Apretude, the injectable option, is administered in a doctor’s office. While these medications are generally safe, mild side effects like nausea, headaches, or fatigue may occur but usually subside over time.
PrEP is highly recommended by the CDC for HIV-negative individuals who meet any of the following conditions:
– Engaged in anal or vaginal sex in the past six months without consistently using condoms.
– Been diagnosed with an STD in the last six months.
– Have an HIV-positive partner.
– Use injection drugs, share needles, or participate in drug treatment programs.
It’s important to note that while PrEP is highly effective against HIV, it does not protect against other sexually transmitted infections (STIs). Safe sex practices, like using condoms and getting regular STI tests, are still essential. For best results, PrEP pills should be taken daily, and follow-up health screenings should be done every two to three months, depending on the form of PrEP being used.
Costs for PrEP can vary, but most insurance plans and Medicaid programs cover it. Generic forms of Truvada, for example, are required to be covered under the Affordable Care Act. Assistance programs are also available for those without coverage, offering free or reduced-cost PrEP options. However, newer medications like Descovy and Apretude may be harder to access due to coverage challenges or prior authorization requirements, creating potential delays in treatment. If you’re considering PrEP, find a provider experienced with these medications to avoid unnecessary complications.
While PrEP is effective, some people avoid it due to stigmas. Misinformation sometimes paints those using PrEP in a negative light, implying promiscuity or reckless behavior. Unfortunately, these misconceptions can discourage individuals from seeking protection. Advocacy groups and the CDC are working to educate the public and improve understanding of PrEP’s benefits.
To start PrEP, talk to your healthcare provider to determine the best HIV prevention plan for you. You’ll need initial testing for HIV, hepatitis B, and other STDs like gonorrhea and chlamydia based on your risk factors. If you face challenges accessing the medication, resources like Planned Parenthood or preplocator.org can help you connect with knowledgeable providers in your area.
In summary, PrEP is a powerful tool for preventing HIV, reducing the risk of transmission by up to 99% when used as prescribed alongside safe sex practices. If you think PrEP might be a good option for you, consult your healthcare provider to begin your prevention journey.